What is Melanoma and How Can I Avoid It?
Melanoma begins in melanocytes, which is the kind of cell that makes the pigment known as melanin. Melanocytes are found in many pigmented tissues, like your skin, eyes, or the intestines. Many cases of melanoma begin in a mole.
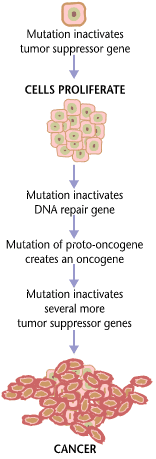
Normal skin cells are produced in the same way every time – healthy cells push old cells to the surface where they are eventually sloughed off. This is part of the reason why your house can get so dusty. Skin cancer develops when skin cells suffer damage due to DNA changes and begin to grow out of control, eventually forming masses of cancerous cells. These masses of cancerous calls are generally called tumors. Scientists still can’t explain exactly what damages skin cells in this way, but they do believe that it’s probably a combination of factors, both genetic and environmental. Scientific studies also suggest that sun exposure and suffering sunburns or sun-induced skin blisters may also play a role in the development of abnormal skin cells that lead to melanoma.
Risk Factors
There are several factors that can increase your risk of getting melanoma:
- Fair skin
- History of sunburns
- Excessive ultraviolet light exposure
- Living close to the equator or at a high elevation
- Having many moles or unusual moles
- A family history of melanoma
- Weakened immune system
Most of these risk factors are related to sun damage and melanin production. There is also an emerging concern that use of erectile dysfunction drugs, such as Viagra, Cialis, or Levitra, may increase your risk of developing melanoma.
Cancer Staging
If you are diagnosed with melanoma, doctors will use a staging scale (from Stage 0 to Stave IV) to describe the cancer. These stages include:
- Stage 0 – This stage is the earliest stage of melanoma. All abnormal melanocytes are in the outer layer of the skin (epidermis). Another name for this stage is “melanoma in situ.” The melanocytes may become cancer and spread into the nearby tissue.
- Stage I – At this stage, it is correct to call the abnormal melanocyte growth cancerous. This stage is divided into two stages. Ulceration is described as a break in the skin. Stage 1 is further defined as follows:
- Stage IA – Not more than 1 millimeter (mm) thick, with no ulceration.
- Stage IB – Not more than 1 mm thick with ulceration, or less than 2 mm thick with no ulceration.
- Stage II – At this stage, the tumor has gone even farther down into the epidermis and has likely broken into the dermis (the layer beneath the outer skin layer). Stage II is further broken down into the following subcategories:
- Stage IIA – More than 1 mm but less than 2 mm thick with ulceration or more than 2 mm but less than 4 mm thick with no ulceration.
- Stage IIB – More than 2 mm but less than 4 mm thick with ulceration or more than 4 mm thick with no ulceration.
- Stage IIC – More than 4 mm thick with ulceration.
- Stage III – At stage III, thickness is no longer a major issue. Instead, this stage is typified by one of the following: the cancer has spread to one or more lymph nodes, the lymph nodes become joined together, the cancer is in a lymph vessel between a primary tumor and nearby lymph nodes, or very small tumors are found under the skin (but no more than 2 cm away from original tumor).
- Stage IV – The cancer has metastasized and spread to other major organs, such as the lungs, GI tract, bone, brain, or liver. Cancer spreads in three ways: through tissues, circulation in the lymph system, and through the bloodstream.
Staging is an important part of being diagnosed with melanoma. The staging matters because it guides doctors in determining which treatments are best for a patient given the particular presentation and severity of their melanoma. Many diagnostic tests are used to determine the staging, and patients may undergo procedures like a simple physical examination, lymph node mapping, CT scans, PET scans, MRIs, and blood tests.
Get Tested
The American Academy of Dermatology recommends that everyone should self-examine their skin each month looking for skin abnormalities and changes. They also recommend that a full-body exam be conducted once a year by a licensed dermatologist.
Performing a self-exam is easy. Check your entire body, including your scalp, palms, the spaces between your toes, and the soles of your feet. Use a hand mirror to visualize areas that are not easily seen. In performing this self-exam, remember A-B-C-D-E, as you are looking for the following characteristics in a mole:
- Asymmetry – the two halves of the mole don’t match
- Border – irregular or poorly defined border on the mole
- Color – the mole has varied coloring, varying shades of tan, brown, or black and sometimes can be red, white or blue
- Diameter – melanomas are typically greater than 6 millimeters, although they can be smaller
- Evolving – a mole that is changing or looks different from your other moles
If you find any moles exhibiting these characteristics, see a dermatologist immediately. Remember, early diagnosis of melanoma or skin cancer can save your life.
Share This



