Drug Induced Progressive Multifocal Leukoencephalopathy (PML)
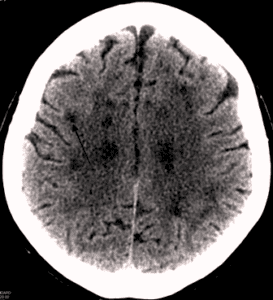
Progressive Multifocal Leukoencephalopathy (PML) is a devastating diagnosis. It is similar to ALS and other progressive neurological diseases that slowly rob patients of their mobility and functioning. PML is caused by a virus that attacks the central nervous system. Once PML has developed, patients quickly experience a decline in their neurological function with loss of coordination, blindness, personality changes, and difficulty speaking. Sadly, the ultimate progression of Progressive Multifocal Leukoencephalopathy is often death.
 Concerns about drug-induced PML first began a few years ago, when the plaque psoriasis drug Raptiva (also known as efalizumab) was linked to a number of Progressive Multifocal Leukoencephalopathy infections. The warning label for Raptiva was updated to reflect this newly-discovered risk in October of 2008 by Genentech. Further changes were made to the warning label for Raptiva in March of 2009, including publication of Medication Guide for patients to help them better understand this very significant risk associated with use of Raptiva. By April of 2009, there were reports of several patients who died of PML after taking Raptiva, which led to the market withdrawal of the drug in June of 2009, which had sales of more than $100 million in 2008. Drug safety organizations also reported that psoriasis patients had developed Guillain-Barre’ Syndrome, Miller Fisher Syndrome, encephalitis, encephalopathy, meningitis, tuberculosis, sepsis, and a number of other serious injuries to patients’ neurological and immune systems.
Concerns about drug-induced PML first began a few years ago, when the plaque psoriasis drug Raptiva (also known as efalizumab) was linked to a number of Progressive Multifocal Leukoencephalopathy infections. The warning label for Raptiva was updated to reflect this newly-discovered risk in October of 2008 by Genentech. Further changes were made to the warning label for Raptiva in March of 2009, including publication of Medication Guide for patients to help them better understand this very significant risk associated with use of Raptiva. By April of 2009, there were reports of several patients who died of PML after taking Raptiva, which led to the market withdrawal of the drug in June of 2009, which had sales of more than $100 million in 2008. Drug safety organizations also reported that psoriasis patients had developed Guillain-Barre’ Syndrome, Miller Fisher Syndrome, encephalitis, encephalopathy, meningitis, tuberculosis, sepsis, and a number of other serious injuries to patients’ neurological and immune systems.
PML has also been reported in patients who have used Tysabri (also known as natalizumab). This drug is marketed by Biogen Idec and Elan Pharmaceuticals and has been prescribed to nearly 100,000 patients with MS. As of October of 2011, the National Multiple Sclerosis Society reported that there have been more than 170 cases of Tysabri-induced PML worldwide with the risks of developing PML being calculated at nearly 2 PML cases per 1,000 patients (with original estimates being only 1 case per 1,000 patients).
RITUXAN (also known as rituximab) is a drug used for various types of Non-Hodgkins Lymphoma (NHL). It is marketed by Biogen Idec and Genentech. A report in a hematology journal in 2009 noted at least 57 patients who had developed PML within three months of taking Rituxan for anemia, rheumatoid arthritis, and lymphoma, and that nearly all of those patients had died as a result of their PML.
One would have hoped that the experience with Raptiva, Tysabri, Rituxan, and others would have been sufficient to avoid future harm to patients. However, in early 2012, there are reports of 2 new cases of PML (in addition to one identified previously) in patients treated with ADCETRIS, also known as brentuximab vedotin. ADCETRIS is approved for use in patients with Hodgkin lymphoma and other lymphomas. Seattle Genetics touts the drug as “the first approved antibody-drug conjugate (ADC) directed to CD30-expressing cells and the first therapeutic advance for HL in 45 years.” The FDA has requested that the risk of PML associated with ADCETRIS be included on a “black box warning,” the highest level of warning for a drug approved by the FDA. There are also concerns about use of ADCETRIS in combination with bleomycin (also known as Blenoxane), as a recent study indicated an increased incidence of pulmonary toxicity in patients treated with this drug combination.
Share This


